Epilepsy is a heterogeneous neurologic condition characterized by an enduring predisposition to recurrent unprovoked epileptic seizures. Epileptic seizures are paroxysmal discharges of excessive hypersynchronous neuronal activity in the brain that lead to transient neurological symptoms by temporarily disrupting normal neuronal functioning and/or inappropriately activating neural pathways. Epileptic seizures may be generalized or focal, depending on whether they begin within a widely distributed bilateral network or within a focal network confined to one hemisphere. Epilepsy is the most common neurological disorder after stroke with an estimated incidence between 40 and 70 per 100,000 person-years. It can have a variety of causes, including metabolic, genetic, or structural, and may occur without identifiable cause or may occur secondary to a known neurological injury such as brain trauma, stroke, or tumor.
The Importance of Psychiatric Symptoms in Epilepsy
Cognitive, emotional, and perceptual symptoms are common in epilepsy, arising from the seizure itself (ictal symptoms), seizure after-effects (post-ictal symptoms), or from persistent abnormalities in brain function independent of seizure activity (inter-ictal symptoms). The prevalence of psychiatric disorders in patients with epilepsy is high with a prevalence of 5.9-55.5% in adults and 24-37% in children. There is a markedly increased prevalence of anxiety, depression, and psychosis relative to the general population. Psychiatric disturbance has a major impact on the quality of life of patients with epilepsy, and depression and anxiety may be among the most important factors predicting a reduced quality of life. We are exploring post-ictal psychiatric symptoms and their relationship to electrical characteristics of seizures. We are also investigating the role of dysfunctional fronto-limbic networks underlying emotional processing in the pathophysiology of inter-ictal depression.
Psychogenic Non-Epileptic Seizures (PNES)
Psychogenic non-epileptic seizures (PNES) are a type of conversion disorder or functional neurologic disorder (FND) that is often mistaken for epilepsy because it is characterized by paroxysmal alterations of awareness, dystonic or myoclonic motor activity, or sensory symptoms much like epilepsy. However, unlike epilepsy, it is not associated with paroxysmal hypersynchronous neural discharges, does not respond to anti-epileptic medications, EEG may be normal during an attack, and psychological causes are generally suspected. PNES is associated with a tendency toward emotional dysregulation, history of psychological trauma, somatization, and dissociation—neuropsychiatric symptom complexes that are believed to predispose patients to these involuntary attacks. Dysfunctional brain circuits mediating emotional expression, regulation and awareness, cognitive control and motor inhibition, self-referential processing, and perceptual awareness are believed to underlie these psychopathologies. The FNL is currently exploring the role of abnormal neural circuit function in patients with PNES.
Weisholtz, D, Khoshbin S. (2016) Psychiatric Manifestations and Treatment of Seizure Disorders. Massachusetts General Hospital Comprehensive Clinical Psychiatry, Second Edition. Ch 77. pp829-838. Stern TA, Fava M, Wilens TE, Rosenbaum JF, eds. Elsevier.
Butler T, Li Y, Twui W, Wang H, Friedman D, French J, Kuzniewcky R, Maoz A, Ichise P, Mozley D, Rusinek H, Vallhabjosula S, Morim S, Thesen T, Talos D, Tanzi E, Harvey P, Glodzik L, Silbersweig D, Stern E, Gauthier S, Mosconi L, Kang Y DeLeon M. Transient and chronic seizure-induced inflammation in human focal epilepsy. Epilepsia (in press)
Perez D, Barsky A, Vago D, Silbersweig DA. A neural circuit framework for somatosensory amplification in somatoform disorders. J Neuropsychiatry Clin Neurosci. 2015. 27(1):40-50. doi: 10.1176/appi.neuropsych.13070170. Epub 2014 Nov 10. Review.PMID: 25716493
Dworetzky BA, Weisholtz DS, Perez DL, Baslet G. (2015) A Clinically Oriented Perspective on Psychogenic Non-epileptic Seizure related Emergencies. Clinical EEG and Neuroscience. 46(1):26-33.
Weisholtz DS, Dworetzky BA. (2014) Epilepsy and Psychosis. J Neurol Disord Stroke. 2(3):1069.
Bui M, Baslet G, Weisholtz D, McElrath T. (2014) Levetiracetam-induced psychosis. Harvard Review of Psychiatry. 22(3):193-200.
Putta S, Weisholtz D, Milligan T. (2014) Occipital seizures and subcortical T2 hypointensity in the setting of hyperglycemia. Epilepsy and Behavior Case Reports. Vol 2:96-99.
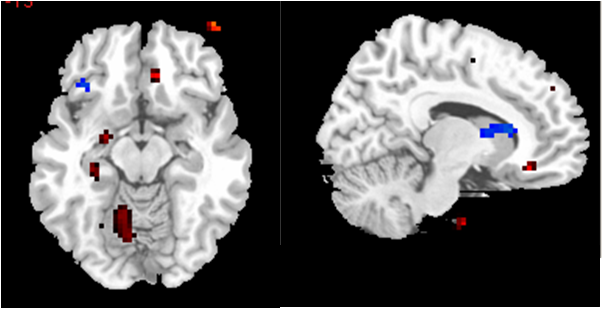
Butler T, Weisholtz D, Isenberg N, Harding E, Epstein J, Stern E, Silbersweig D. Neuroimaging of frontal-limbic dysfunction in schizophrenia and epilepsy-related psychosis: Toward a convergent neurobiology. Epilepsy & Behavior 2012 Feb;23(2):113-22. Epub 2011 Dec 29.
Perez D, Barsky A, Daffner K, Silbersweig D. Motor and somatosensory conversion disorder; a functional unawareness syndrome? J Neuropsychiatry Clin Neuroscs, 24: 141-151, 2012.
Butler T, Ichise M, Teich A, Osborne J, French J, Devinsky O, Kuzniecky R, Gilliam F, Pervez F, Provenzano F, Goldsmith S, Vallabhajosula S, Stern E, Silbersweig DA. Imaging inflammation in a patient with epilepsy due to focal cortical dysplasia. J Neuroimaging 2011; . [ DOI ]
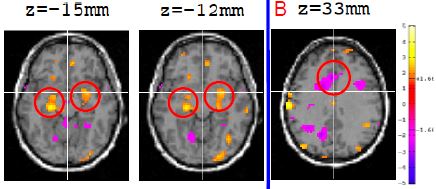
Butler T, Pan H, Pavony M, Xie XH, Ponticello L, Kandula P, Harden C, Labar D, Stern E, Silbersweig D. Resting state hippocampal functional connectivity in temporal lobe epilepsy. Epilepsia 2007; 48:152-153.
